Upper Extremity DVT- April Case of the Month
Upper Extremity DVT
Case: A 37-year-old female presented to the emergency department with a unilateral swollen left arm, and some pain in the axillary spreading down to the elbow. She had noticed the swelling for 3 weeks. She had a picc line removed 2 weeks prior. She had this placed for antibiotics to treat an osteomyelitis which had presumably resolved. She had mentioned the swelling and pain to the specialist at the time of Picc line removal, but they were not concerned. As the swelling and pain worsened, she presented to the ER department. Her vital signs were normal. On exam she was neuro-vascularly intact on the left upper extremity, however it was uniformly swollen, with tenderness in the axilla. As a DVT was suspected, we grabbed the POCUS probe and got to scanning.
The Upper Extremity DVT scan: POCUS can be an effective tool in elucidating the cause of a unilateral swollen vein, even in the upper extremity. The use of POCUS for lower extremity DVT is extremely sensitive and specific when used by emergency medicine physicians (1). However, UE DVT is rarer, and hasn’t been specifically studied, but the same principles in POCUS diagnostics apply, and it can be an effective tool to help diagnose and treat in a timely fashion (2).

Anatomy review:
From Wikipedia
Target Veins: The deep veins of the upper extremity are the subclavian vein, the axillary vein, and the brachial veins (3). These can be scanned in any order. Figure out what works best for you. It is important that you scan them all though.
- Internal jugular (IJV)
- Subclavian
- Axillary
- Brachial (paired)
Positive DVT Indicators:
- Incomplete/absent compressibility
- Echogenic material in vein
- Absent or non-phasic Doppler flow
- No augmentation with distal squeeze
Upper Extremity DVT POCUS Scan – Step-by-Step
Preparation:
- Explain procedure, obtain consent.
- Position: supine or semi-recumbent, arm abducted slightly.
- Use high-frequency linear probe (5–15 MHz) with venous/vascular preset.
Scanning Technique:
- Internal Jugular Vein:
- Transverse view at neck.
- Identify IJV (lateral) and carotid artery (medial).
- Compress: vein should fully collapse.
- Optional: use color Doppler or augment with distal compression.
- Subclavian Vein:
- Probe infraclavicular, longitudinal view is often necessary but can view parts in transverse.
- Cannot compress due to clavicle.
- Use color Doppler to assess flow and respiratory variation.
- Look for thrombus or absent flow.
- Can also use pulse wave to determine if there is no biphasic flow.
- Axillary Vein:
- Slide probe laterally/inferiorly from subclavian.
- Transverse view: vein is medial/anterior to artery.
- Compress every 1–2 cm.
- Brachial Veins:
- Continue distally down arm.
- Identify paired veins around brachial artery.
- Compress every 1–2 cm.
- Check for compressibility and thrombus.
Back to our case:
IJ Views (Click on image for video)
The IJ was fully compressed at baseline, and a Valsalva maneuver was required to obtain adequate images of the IJ. No DVT was present.
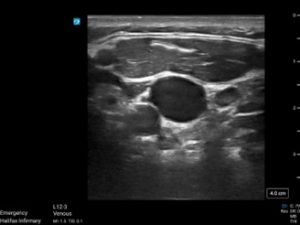
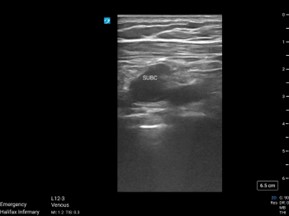
Subclavian views (Click on images for both videos)
Adequate images were obtained in the transverse view before the branching of the cephalic and axillary vein.
There was visible clot present in the subclavian vein, noted by the increased echogenicity within the vein. The vein was not compressible. There was also no flow, suggesting clot presence.
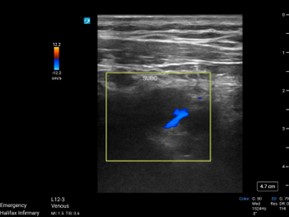
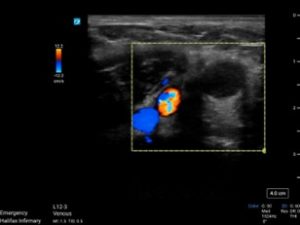
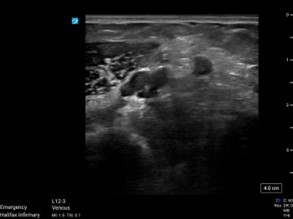
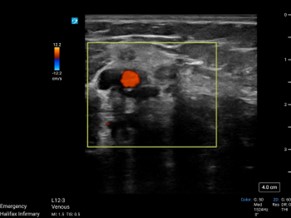
Axillary Vein (Click on images for both videos)
The axillary vein was obtained with the probe in the axilla, with compression then color flow
Axillary vein to the R of the image demonstrated echogenicity, non-compressibility, and no flow, indicating clot presence.
Brachial vein to the R also demonstrated no compressibility or flow.
Brachial Vein(Click on images for both videos)
Case Resolution and Discussion:
The patient was started on DOAC, and then a formal ultrasound was ordered, which confirmed clot was present in the subclavian, axillary, and brachial veins of the left upper extremity. There was also clot in the basilic vein. The patient was prescribed anticoagulation, and an appointment for follow up. DVT of the upper extremity is rare and is classified as primary vs secondary. Primary, aka Paget Schroetter syndrome (PSS), occurs in young athletes who use one their arms in repetitive movements (volleyball, gymnastics, swimming, ball throwing sports). Secondary occurs with malignancy or deep vein catheterization. If a catheter is in place, then the site should be assessed for infection as well. There is less evidence on how to manage them compared to lower extremity DVT’s due to their rarity. Thrombosis guidelines advise to treat like DVT’s of the lower extremity (4). There is some concern of using DOACs with catheters in situ, due to the belief that they may not be as effective with a foreign body (5). However, the trend amongst providers is to use DOACs, and there is preliminary evidence suggesting they are as effective, with more studies being done (5).
Take Home Points:
- POCUS can be an effective tool in diagnosing both upper and lower extremity DVTs
- Upper extremity scans require visualizing the IJ, the subclavian, the axillary, and brachial veins.
- Check for visible clot, compressibility, and color flow. Pulse wave and augmented flow can be used to aid when these are inconclusive or difficult to obtain.
- Treat UE DVTs as LE DVTs with anticoagulation as recommended by specialty consensus groups. (Thrombosis Canada)
References:
- Pomero F, Dentali F, Borretta V, et al. Accuracy of emergency physician-performed ultrasonography in the diagnosis of deep-vein thrombosis: a systematic review and meta-analysis. Thromb Haemost. 2013;109(1):137-145.
- Schafer JM, Stickles S. Deep Vein Thrombosis (DVT). ACEP Sonoguide. American College of Emergency Physicians. Published August 18, 2020. Accessed April 17, 2025. https://www.acep.org/sonoguide/basic/dvt/
- Grigorian A, Nahmias JT. Upper Extremity Deep Venous Thrombosis. In: StatPearls. StatPearls Publishing; 2023. Accessed April 17, 2025. https://www.ncbi.nlm.nih.gov/books/NBK482420/
- Thrombosis Canada. (2023). Deep Vein Thrombosis: Treatment. Retrieved April 17, 2025, from https://thrombosiscanada.ca/hcp/practice/clinical_guides?guideID=DEEPVEINTHROMBOSISTREATMENT&language=en-ca
- Bosch, F. T. M., Di Nisio, M., Büller, H. R., & van Es, N. (2020). Diagnostic and therapeutic management of upper extremity deep vein thrombosis. Journal of Clinical Medicine, 9(7), 2069. https://doi.org/10.3390/jcm9072069